HOUSTON, TX / ACCESSWIRE / April 14, 2023 / In many ways, Alzheimer's disease (AD) remains a mystery. Most common in those over 65, AD is the most common form of dementia, but its exact causes remain unclear, and treatments are unable to halt or reverse disease progression. What is clear is the urgency of developing proper treatments for the disease.
The human and social costs of AD are becoming more and more apparent. There are currently around 6 million citizens with AD, and that number is expected to reach almost 13 million by 2050. Within the same time frame, the costs to America from AD and other types of dementia are predicted to skyrocket from $345 billion to almost $1 trillion. As many as one in every three citizens dies with AD or another dementia.
While AD is currently still irreversible, investment in research and development (R&D) around the disease is at an all-time high. The global market for AD treatment is predicted to reach $6.3 billion by 2029, and there are more AD drug candidates in development than ever before.
Some drugs approved by the Food and Drug Administration (FDA) focus on alleviating some of the cognitive symptoms, like memory loss. Others are disease-modifying treatments that use anti-amyloid therapies to target the toxic build-up of the beta-amyloid protein in the brain. Research is affirming the latter approach to tackling amyloid accumulation - there are indications that treatments that support the immune system could reduce the build-up of amyloid protein and even prevent disease progression.
Treg Therapy: How The Immune System Can Combat AD
Microglia is the specialized type of immune cell that prevents toxic chemicals from collecting in the brain. However, as AD progresses, amyloid protein builds up in the brain, and the plaque overwhelms the immune cells and stops them from functioning. This can even cause the dysfunctional microglia to turn on the brain and increase neurodegeneration and inflammation.
Recent research suggests that this collapse of the immune response might be prevented, and AD progression slowed, by targeting the cellular system that modulates inflammation. This immunotherapy promotes regulatory t-cell (Treg) function, the cells that regulate the immune system and work in an anti-inflammatory capacity. Treg cell therapy has caught the attention of leading biopharma companies like Eli Lilly and Company and Novartis, which have both invested in companies developing Treg-based treatments.
Coya Therapeutics To Release Data On Treg Drug Candidates
Preliminary research suggests that modified Treg cells can indeed boost the response of microglia, down-regulating inflammation and fighting off amyloid protein build-up. This is an exciting development, as it suggests that targeted support of the immune system via Treg treatment could help the brain slow or even halt AD progression. Coya Therapeutics (NASDAQ:COYA) is a clinical-stage biotechnology company that is leading the field in developing Treg therapies.
Part of Coya's development pipeline is the Treg-enhancing biologic, COYA 301. COYA 301 aims at reducing neuroinflammation by supporting the development, expansion and activity of Treg cells in the brain. The company will release clinical data in mid-May illustrating the preliminary COYA 301's efficacy and biomarkers for eight patients with AD.
The company has a pipeline of other Treg-enhancing therapies, including COYA 302 for treating amyotrophic lateral sclerosis (ALS), and COYA 101, which has validated its therapeutic approach through multiple trials.
Visit its website to dive deeper into Coya Therapeutic's exciting work at the frontier of Alzheimer's treatment.
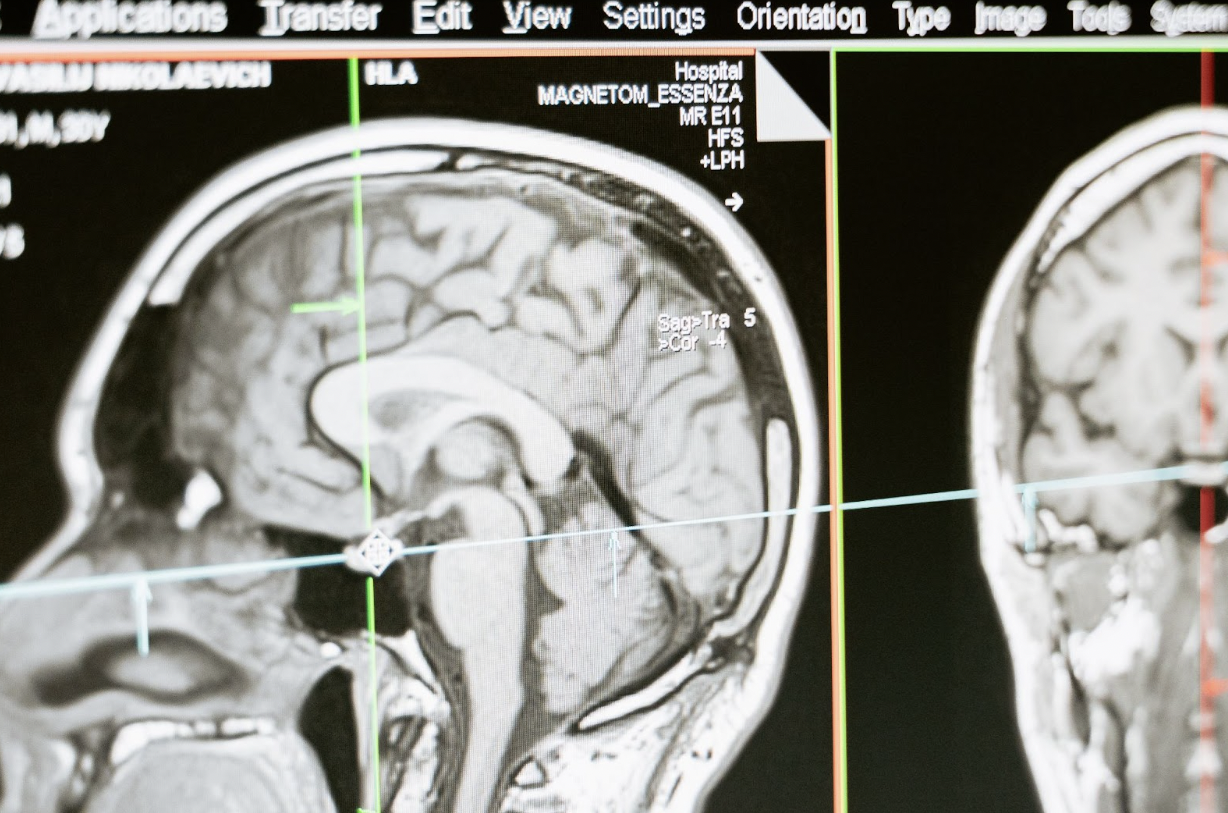
Featured photo by MART PRODUCTION on Pexels
Contact:
David S. Snyder
David@coyatherapeutics.com
SOURCE: Coya Therapeutics Inc.
View source version on accesswire.com:https://www.accesswire.com/749246/Alzheimers-Disease-Largely-Remains-A-Mystery-With-A-Lack-Of-Highly-Effective-Treatments--Could-Regulatory-T-Cells-Tregs-Be-The-Answer
